Spondylitis: Types, symptoms, diagnosis, and treatment - Medical News Today
Spondylitis is an umbrella term for a group of chronic arthritis-type diseases affecting the joints of the spine and sacroiliac region. The sacroiliac region includes the pelvis and lower spine.
Medical professionals categorize spondylitis into different subtypes. Some subtypes cause widespread inflammation that may affect multiple organs or systems within the body.
This article describes what spondylitis is and how it differs from a similar condition called spondylosis. We then outline the different types of spondylitis and their associated causes and symptoms. Finally, we provide information on diagnosing and treating spondylitis.
Spondylitis is an umbrella term for a group of chronic arthritis-type diseases affecting the joints of the spine and sacroiliac region.
All types of spondylitis involve inflammation of the joints, tendons, and ligaments. Tendons are connective tissues that attach muscle to bone, while ligaments are connective tissues that attach bones to other bones.
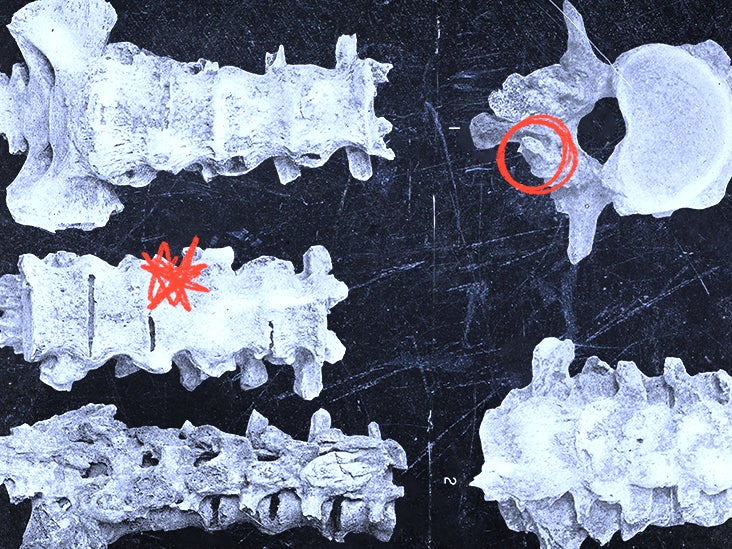
Inflammation of the joints can cause bones to fuse and trigger excessive bone growth in the spine. Severe cases can cause excessive curvature of the spine.
Spondylitis and spondylosis are similar conditions that can both cause hip and back pain. However, the two conditions have different characteristics and causes.
Spondylitis
Spondylitis is a condition in which the immune system attacks the joints, causing inflammation, bone fusion, and excess bone formation.
Certain types of spondylitis tend to develop in teenagers and young adults.
Spondylosis
Spondylosis is a type of arthritis related to aging and general wear and tear of the spine. It occurs when the joints and discs of the spine degenerate. Osteophytes, which are bone spurs that grow on the individual backbones or vertebrae, may also cause it.
Spondylosis tends to affect older people. More than 85% of people over the age of 60 have the condition.
Doctors may use two different classification systems when diagnosing spondylitis: the traditional system and the newer system. According to the Spondylitis Association of America, the traditional system recognizes six types of spondylitis, while the newer system consists of two broader categories encompassing all types of spondylitis.
Traditional spondylitis classifications
The traditional spondylitis classification system categorizes spondylitis into six types. These are:
Ankylosing spondylitis
Ankylosing spondylitis (AS) is a form of chronic joint inflammation that primarily affects the spine. The term "ankylosis" refers to joint stiffness resulting from injury or disease. In AS, a fusion of the spinal vertebrae causes stiffness and limited movement in the spine.
AS usually begins during the teenage years or in early adulthood.
Symptoms
Symptoms of AS may develop slowly over time and may come and go. They may include:
Causes
Experts do not know the exact cause of AS. However, 9 out of 10 people who have AS carry the gene human leukocyte antigen B27 (HLA-B27).
This suggests that the gene may predispose a person to AS but does not mean that a person with the gene will develop the condition. Researchers estimate that 8 in every 100 people have the HLA-B27 gene, but most do not develop AS.
Reactive arthritis
Reactive arthritis (ReA) is a type of inflammatory arthritis that typically presents several days or weeks following a gastrointestinal infection or sexually transmitted infection (STI).
Experts sometimes describe ReA as a triad of inflammatory conditions, though
Symptoms
Symptoms of ReA may include:
- Arthritis: Swelling and pain in the joints.
- Conjunctivitis: Inflammation of the eyes accompanied by a sticky discharge.
- Urethritis: Genital and bladder inflammation and pain while urinating.
Causes
Reactive arthritistypically results from a bowel infection or certain STIs. People may also develop ReA following a bout of glandular fever or erythema infectiosum.
In ReA, the immune system overreacts to infection and begins attacking healthy tissues. This leads to inflammation.
Research also links reactive arthritis to the HLA-B27 gene. Scientists estimate that
Psoriatic arthritis
Psoriatic arthritis (PsA) is a chronic inflammatory disease that affects the joints and areas where ligaments and tendons attach to bone. The disease is associated with the inflammatory skin condition psoriasis. For many people, PsA develops about 10 years after psoriasis, but some people develop PsA first or without ever having psoriasis.
Psoriatic arthritis can present at any age but typically affects people aged 30–50.
Symptoms
Symptoms of PsA may include:
Causes
A person may develop PsA in a joint following an injury. The disease may also have a genetic link. Researchers estimate that at least 10% of the population inherits one or more genes that predispose a person to psoriasis.
Enteropathic Arthritis
Enteropathic arthritis (EnA) is a type of chronic inflammatory arthritis associated with inflammatory bowel diseases (IBDs), such as ulcerative colitis (UC) and Crohn's disease (CD). Approximately 1 in 5 people with UC or CD also develop EnA.
Enteropathic arthritis typically affects joints in the arms, legs, and spine.
Symptoms
The symptoms of EnA may include those related to IBD, as well as those related to arthritis. Examples include:
Causes
Experts do not know the precise cause of EnA but believe the disease is associated with inflammation in the bowel. Chronic bowel inflammation may allow bacteria to enter the damaged bowel wall and move through the bloodstream. The body's reaction to these bacteria may cause further inflammation and pain.
Enteropathic arthritis is also associated with the gene "HLA-B27".
Juvenile spondyloarthritis
Juvenile spondyloarthritis is chronic inflammatory arthritis that begins in people aged
Symptoms
Symptoms of JSpA may
Causes
Experts do not know the precise cause of JSpA. However, as with spondylitis in adults, children with the disease often carry the HLA-B27 gene.
Undifferentiated spondyloarthritis
Undifferentiated spondyloarthritis (USpA) is a diagnosis a doctor may give when a person presents with a variety of symptoms that doctors cannot classify as a specific rheumatoid disorder.
Symptoms
Symptoms of USpA vary but may include:
- persistent pain in the lower back, which develops before age 45
- joint pain in small and large joints
- heel pain
- swelling in the hands and feet
- general stiffness
- inflammation of the eye
- bumpy rash
- urinary tract and genital symptoms, such as pain and discharge
- intestinal inflammation
- diarrhea
Newer spondylitis categorizations
The newer spondylitis classification system categorizes spondylitis into two main types according to where in the body the disease occurs. The two types are peripheral spondyloarthritis and axial spondyloarthritis.
Peripheral spondyloarthritis
Peripheral spondyloarthritis (pSpA) typically causes inflammation in the joints and tendons outside the spine and sacroiliac joints. The disease usually affects the following areas:
- hands
- wrists
- elbows
- shoulders
- knees
- ankles
- feet
A person with pSpA may experience dactylitis, which is inflammation of the toes and fingers, or enthesitis, which is inflammation in areas where ligaments and tendons attach to bone.
This category includes the following forms of spondylitis:
- reactive arthritis
- enteropathic arthritis
- undifferentiated arthritis
Axial spondyloarthritis
Axial spondyloarthritis (AxSpA) causes inflammation and pain in the pelvis, the spine, or both. This category covers a broad range of spondylitis types and includes people with and without sacroiliac joint fusion and damage.
There is no definitive test to diagnose spondylitis. Doctors will carry out a physical examination that includes questions about a person's symptoms and medical history. They will also ask if the person has a family history of autoimmune diseases, including psoriasis and spondyloarthritis.
Diagnosis may also involve the following:
- blood tests
- imaging tests, such as:
- genetic testing for the HLA-B27 gene
There is no cure for spondylitis. However, treatments can help manage the condition and alleviate symptoms.
Treatment options may include the following:
- medications to reduce inflammation and pain, such as:
- physical therapy, which may include massage and spinal manipulation to improve and maintain spine flexibility
- exercises to alleviate joint pain and stiffness
- breathing exercises to ensure normal chest expansion
In some cases, doctors may also recommend surgery to repair severely damaged joints or correct extreme curvature of the spine. However, surgery for spondylitis is rare compared with other treatment approaches.
A person may use complementary therapies alongside standard spondylitis treatments for added symptom relief. These therapies may
Spondylitis refers to a group of inflammatory, arthritis-type diseases. The traditional spondylitis categorization system recognizes six subtypes of spondylitis. The newer categorization system recognizes two broader subtypes according to the area of the body the disease affects.
There is no official diagnostic test for spondylitis. Instead, a doctor may use a combination of tests to diagnose the disease. These may include blood tests, imaging tests, and genetic testing.
While there is no cure for spondylitis, treatments may help manage the disease and alleviate symptoms. Treatment options include medications, physical therapy, and exercises. Some people may also wish to try complementary therapies such as massage, relaxation techniques, and acupuncture alongside standard treatments.
Comments
Post a Comment