How a Common Stomach Bug Causes Cancer - The Atlantic
At first, doctors didn't believe that bacteria could live in the stomach at all. Too acidic, they thought. But in 1984, a young Australian physician named Barry Marshall gulped down an infamous concoction of beef broth laced with Helicobacter pylori bacteria. On day eight, he started vomiting. On day 10, an endoscopy revealed that H. pylori had colonized his stomach, their characteristic spiral shape unmistakable under the microscope.
Left untreated, H. pylori usually establishes infections that persist for an entire lifetime, and they're common: Half of the world's population harbors H. pylori inside their stomach, as do more than one in three Americans. In most cases, the microbe settles into an asymptomatic chronic infection, but in some, it becomes far more troublesome. It can, for example, cause enough damage to the stomach lining to create ulcers. Worse still, H. pylori can lead to cancer. This single bacterium is by far the No. 1 risk factor in stomach cancers worldwide. By one estimate, some 70 percent can be attributed to H. pylori.
But what still puzzles doctors years later is why H. pylori has such different consequences for different people. Why is it asymptomatic in most but carcinogenic in others? Although the full answer is complex, one key factor seems to be mutations in H. pylori itself. Not every strain is created equal. The presence of select genes intensifies H. pylori's pathogenicity, and even a single mutation in a single gene, scientists recently found, enhances the link to cancer. A small genetic tweak in a common stomach bug could have profound consequences for us, its unwitting hosts.
H. pylori has lived inside of us for a long time. Our ancestors who left Africa likely carried it inside them as they crossed continents and oceans, built and felled civilizations. And over the course of what some scientists hypothesize to be more than 100,000 years of co-evolution, H. pylori has exquisitely adapted to the harsh, acidic conditions of the human stomach.
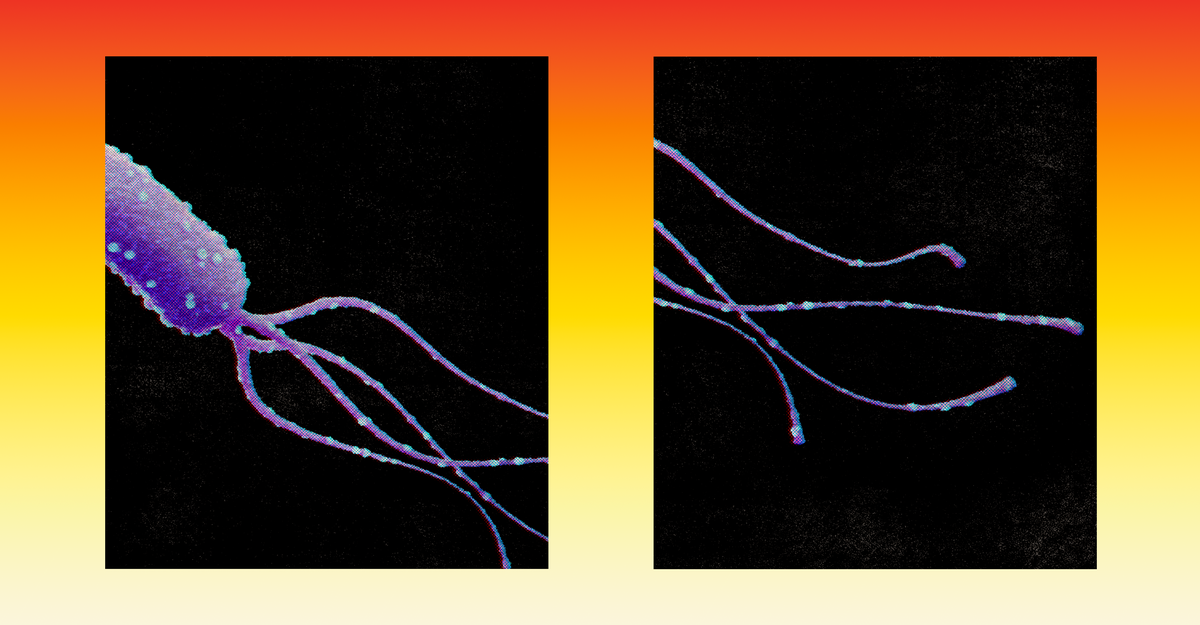
It survives, for example, by producing "copious amounts" of an enzyme that neutralizes stomach acid, Richard Peek, a gastroenterologist at Vanderbilt, told me. H. pylori can also burrow into the mucus-gel lining of the stomach using powerful, whiplike flagella. The mucus lining offers a relative haven from stomach acid, but another prize lies underneath too: stomach cells, rich in nutrients that the bacteria needs to survive.
The way that H. pylori steals nutrients could be the key to how it ends up causing cancer. The bacterium isn't necessarily out to hurt its human host. "H. pylori doesn't want you to get an ulcer or to get cancer, but it needs to replicate to high enough levels in the stomach that it can be transmitted to another person," Nina Salama, a biologist at Fred Hutchinson Cancer Center, told me. (The bacteria seem to spread through an infected person's saliva, vomit, or feces.) But to replicate, it needs nutrients, in particular iron, which our cells probably hoard to starve pathogens.
In response, certain strains of H. pylori have evolved genetic changes that might make its iron-mining more efficient. But this also causes more collateral damage to the host's stomach, enough damage, perhaps, to eventually trigger cancer. First, the bacteria uses a protein called HtrA—essentially "a pair of molecular scissors," Peek said—to cut the bonds that hold stomach cells together, so the microbes can slip between. A single mutation in this scissor protein makes it better at cutting, a group based in Germany found in a recent study, and this mutation is disproportionately found in H. pylori strains isolated from people who developed stomach cancer.
Once H. pylori has wedged itself in between cells, it also has clever ways of accessing the nutrients inside. Certain strains carry a set of about 18 genes that collectively encode a molecular needle through which H. pylori injects bacterial proteins, triggering a cascade of changes to the cell. These hijacked cells end up giving up their iron more easily, but they also become worse at essential functions such as fixing damaged DNA. This set of approximately 18 genes, collectively called the "cag pathogenicity island," are in fact disproportionately found in strains from cancer patients. Stomach cancer thus might be a secondary consequence of the microbe's aggressive search for nutrients. For the H. pylori, "there's no selective pressure to cause cancer in 80 years. The selective pressure is to acquire iron now," Karen Guillemin, a microbiologist at the University of Oregon, said.
But not everyone infected with one of these cancer-linked strains will develop cancer. Other factors likely play a role too: diet, environment, and genetics of the individual patient Stomach-cancer rates vary quite widely around the world, with the highest prevalence in East Asia. In Japan, doctors routinely test for H. pylori in people with no symptoms, and prescribe antibiotics if the tests come back positive. But some scientists have argued against aggressive treatment, pointing at hints that humans derive some benefits from living with H. pylori too. Those infected, for example, tend to have lower rates of asthma and allergy. Genetic signatures associated with more pathogenic H. pylori strains, Peek told me, would help identify those at highest risk, who could most benefit from antibiotics.
Marshall, the Australian doctor who infected himself with H. pylori, ultimately recovered just fine. His self-experiment, in addition to other studies with his collaborator Robin Warren, proved that the bacterium does indeed infect the stomach and does indeed cause stomach ulcers, which later spurred the work linking H. pylori to cancer. Understanding exactly how and why H. pylori becomes pathogenic is still key to finding the way to treat it, but in the past 40 years the significance of H. pylori to human health has become indisputable—so much so that in 2005, Marshall and Warren won the Nobel Prize in Medicine.
Comments
Post a Comment