Experts Alert Doctors & the Public to the Arrival of Hard-to-Treat Fungal Skin Infections in the U.S. - NYU Langone Health
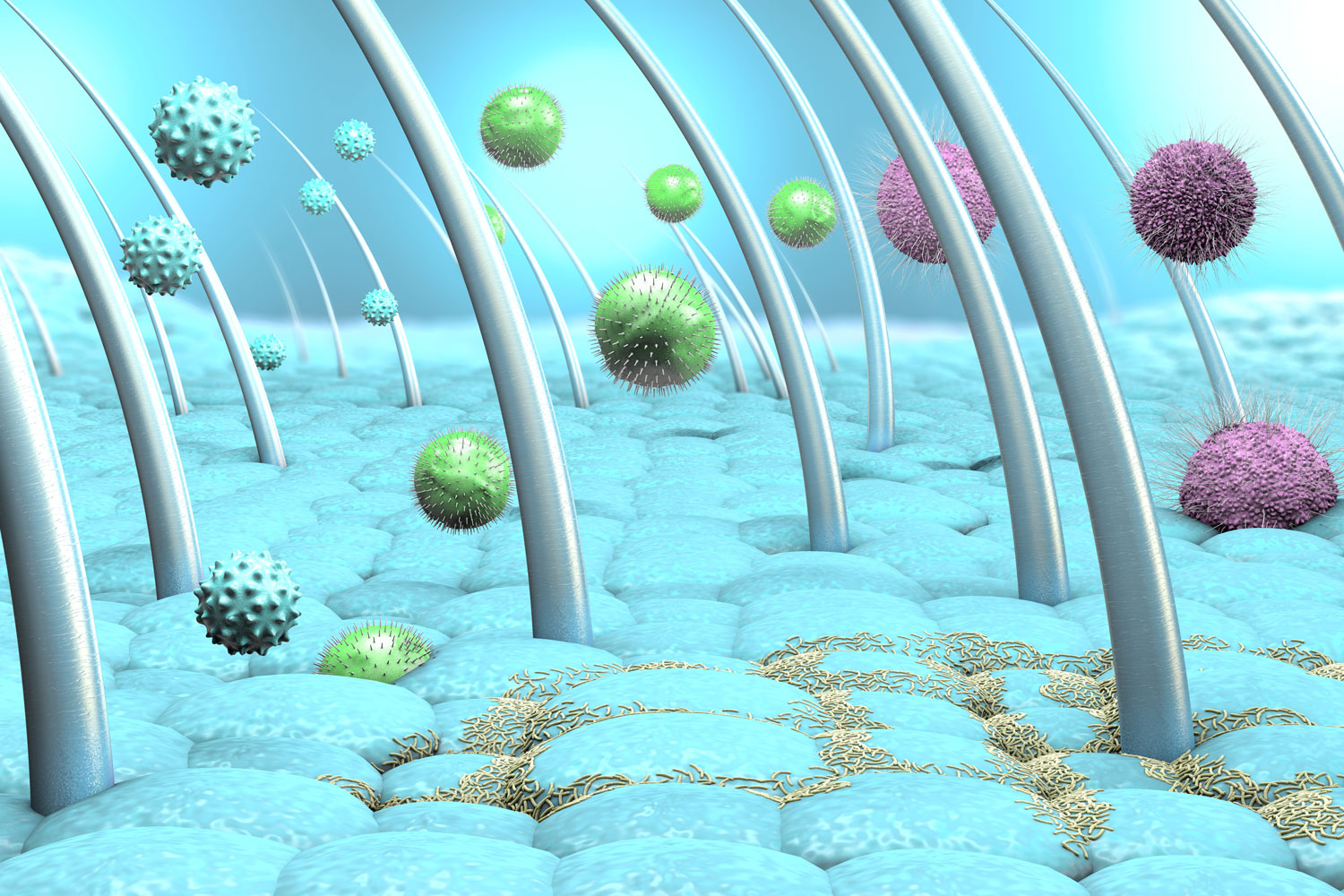
Healthcare providers should watch out for new and highly contagious forms of ringworm or jock itch, which are emerging as a potential public health threat, according to a pair of reports.
In the first of the studies, experts at NYU Langone Health who focus on the spread of contagious rashes document the first reported case in the United States of a sexually transmitted fungal infection that can take months to clear up, even with treatment. In the second report, NYU Langone physicians partnered with authorities at the New York State Department of Health to describe the largest group of patients in the country with a similar fungal strain that resists standard therapies.
Both species of fungi are among a group that causes skin rashes, or tinea, which easily spread on the face and limbs (ringworm), groin (jock itch), and feet (athlete's foot). However, the tinea explored in the new reports can look very different from the neat, regular circles seen in most forms of ringworm. They may instead be confused for lesions caused by eczema and can therefore go without proper treatment for months.
The first report, which published online on June 5 in the journal JAMA Dermatology, describes a man in his 30s who developed tinea on his penis, buttocks, and limbs after returning home to New York City from a trip to England, Greece, and California. Genetic tests of fungal samples collected from the patient's rashes revealed that the infection was caused by the species Trichophyton mentagrophytes type VII (TMVII). This sexually transmitted form of ringworm has been increasingly diagnosed throughout Europe, with 13 instances reported in France in 2023, mostly in men who have sex with men. Notably, the man in the current study said he had sex with multiple male partners during his travels, none of whom reported similar skin issues.
"Healthcare providers should be aware that Trichophyton mentagrophytes type VII is the latest in a group of severe skin infections to have now reached the United States," said study lead author and dermatologist Avrom S. Caplan, MD. Dr. Caplan is an assistant professor in the Ronald O. Perelman Department of Dermatology at NYU Grossman School of Medicine.
"Since patients are often reluctant to discuss genital problems, physicians need to directly ask about rashes around the groin and buttocks, especially for those who are sexually active, have recently traveled abroad, and report itchy areas elsewhere on the body," added study senior author John G. Zampella, MD.
Dr. Zampella, an associate professor in the Ronald O. Perelman Department of Dermatology, says that while infections caused by TMVII are difficult to treat and can take months to clear up, they so far appear to respond to standard antifungal therapies, such as terbinafine.
Meanwhile, Dr. Caplan says the new skin condition explored in his other new report presents a greater challenge for dermatologists. The study results, published online in May in JAMA Dermatology, center on Trichophyton indotineae, which is widespread in India and is now reported globally. First confirmed in the United States last year, the infection causes itchy and contagious rashes similar to those of TMVII, but it often resists terbinafine treatment.
To better understand how T. indotineae can evade antifungal drugs, the researchers collected clinical and laboratory data from 11 men and women treated for ringworm in New York City hospitals between May 2022 and May 2023. Their tinea was confirmed to have been caused by T. indotineae. Seven of the patients had received standard doses of terbinafine for anywhere from 14 days (the usual duration for most forms of ringworm) to 42 days, yet their rashes did not improve.
Analyzing the fungal samples' DNA, the team reported several variations in the genetic code (mutations) that prevent terbinafine from hooking onto fungal cells and poking holes in their protective membranes. According to the study authors, these mutations might help explain why the therapy often failed in some cases to fight the infections.
The results also showed that when seven patients were treated with another antifungal called itraconazole, three recovered entirely and two improved. The problem with this therapy, Dr. Caplan says, is that while effective, the drug can interfere with many medications and can cause nausea, diarrhea, and other side effects that make it hard to use for long periods.
"These findings offer new insight into how some of the fungal skin infections spreading from South Asia can evade our go-to therapies," said Dr. Caplan. "Beyond learning to recognize their misleading signs, physicians will need to ensure their treatment addresses each patient's quality of life needs."
Dr. Caplan adds that he plans to work with leading fungi experts around the United States and internationally over the next few months to expand research efforts and track emerging cases.
The researchers caution that while dermatologists should be on the alert for signs of TMVII and T. indotineae in their patients, rates so far remain low in the United States.
Study funding was provided by NYU Langone.
In addition to Dr. Caplan and Dr. Zampella, other NYU Langone investigators involved in the TMVII study are Michelle Sikora, BS; Arianna Strome, MD; Christine Akoh, MD, PhD; and Caitlin Otto, PhD. Other study authors include Sudha Chaturvedi, PhD, at the New York State Department of Health in Albany.
Besides Dr. Caplan, other NYU Langone researchers involved in the T. indotineae study are Michelle Sikora, BS, and Christine Akoh, MD, PhD. Other study authors include Gabrielle Todd, PhD; YanChun Zhu, MS; Swati Manjari, PhD; and Nilesh Banavali, PhD; at the New York State Department of Health in Albany; and Jeannette Jakus, MD, MBA; Shari Lipner, MD, PhD; Kayla Babbush, MD; Karen Acker, MD; Ayana Morales, MD; Rebecca Marrero Rolon, MD; Lars Westblade, PhD; Maira Fonseca, MD; and Abigail Cline, MD, PhD; at Weill Cornell Medicine in New York City.
Further study authors were Jeremy Gold, MD, MS; Shawn Lockhart, PhD; Dallas Smith, PharmD; and Tom Chiller, MD, at the U.S. Centers for Disease Control and Prevention in Atlanta; and William Greendyke, MD, at the New York City Department of Health and Mental Hygiene. Sudha Chaturvedi, PhD, served as study senior author.
Media Inquiries
Shira Polan
Phone: 212-404-4279
Shira.Polan@NYULangone.org
Comments
Post a Comment